

Resources
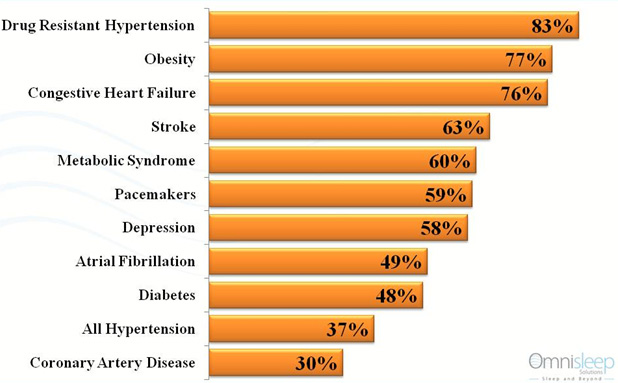
Sleep Apnea in Comorbidities
- Almost 50% of type 2 diabetes patients have sleep apnea.
Prevalence of sleep apnea in the population of adults with type 2 diabetes mellitus. Einhorn et al. Endocrince Practice, 2007. View article - Among obese type 2 diabetes patients, the prevalence of sleep apnea has been estimated at 86%.
Obstructive sleep apnea among obese patients with type 2 diabetes. Foster et al. Diabetes Care, 2009. View article - Insulin responsiveness increased 28% in patients with type 2 diabetes after 4 months of apnea treatment.
Obstructive sleep apnea in obese noninsulin-dependent diabetic patients: effects of continuous positive airway pressure treatment on insulin responsiveness. Brooks et al. Journal of Clinical Endocrinology and Metabolism, 1994. View article
- Obstructive sleep apnea syndrome increases the risk of stroke, independent of other risk factors
• Risk of stroke doubles in men with mild sleep apnea
• Risk of stroke triples in men with moderate to severe sleep apneaObstructive sleep apnea as a risk factor for stroke and death. Yaggi et al. New England Journal of Medicine, 2005. View article
Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: The sleep heart health study. Gottlieb et al. Circulation, 2010. View article
- Impaired attention, memory, and executive function (eg, problem-solving) may intensify with increasing apnea severity.
The effect of sleep fragmentation on daytime function. Martin et al. American Journal of Respiratory and Critical Care in Medicine. 1996. View article
- People with untreated sleep apnea are less alert and vigilant, with poorer attention than healthy control subjects.
Daytime variation in performance and tiredness/sleepiness ratings in patients with insomnia, narcolepsy, sleep apnea and normal controls. Schneider et al. Journal of Sleep Research, 2004.View article
- OSA was associated with an increased risk of depression – depression symptoms were seen in 35% of OSA patients and 8% of controls.
Depression, sleepiness, and disease severity in patients with obstructive sleep apnea. Ishman SL, Laryngoscope, 2010. View article
OSA may create vulnerability to insomnia and mood disorders 2. Complex insomnia: insomnia and sleep-disordered breathing in a consecutive series of crime victims with nightmares and PTSD. Krakow et al. Biological Psychiatry, 2001. View article
- Apnea treatment results in a clinically significant drop in blood pressure of up to 10 mm mercury. This drop is sufficient enough to reduce the risk of a coronary heart disease event by 37% and stroke risk by 56%.
Refractory hypertension and sleep apnoea: effect of CPAP on blood pressure and baroreflex. Logan et al. European Respiratory Journal, 2003. View article
Effect of nasal continuous positive airway pressure treatment on blood pressure in patients with obstructive sleep apnea. Becker et al. Circulation, 2003. View article
Ambulatory blood pressure after therapeutic and subtherapeutic nasal continuous positive airway pressure for obstructive sleep apnoea: a randomised parallel trial. Pepperell et al. Lancet, 2002. View article
- Severe apnea sufferers have a 46% increased risk of mortality.
Sleep-Disordered Breathing and Mortality: A Prospective Cohort Study. Punjabi et al, PLoS Medicine, 2009. View article
- The worse the patient apnea, the greater the risk of developing hypertension and other forms of cardiovascular diseases.
Obstructive sleep apnea syndrome as a risk factor for hypertension: a population study. Lavie et al. British Medical Journal, 2000. View article
- Coronary artery disease patients with obstructive sleep apnea have fewer deaths and hospitalizations over 5 years when their apnea is treated.
Benefits of obstructive sleep apnoea treatment in coronary artery disease: a long-term follow-up study. Milleron et al. European Heart Journal, 2004. View article - 76% of heart failure patients have sleep-disordered breathing.
Sleep-disordered breathing in patients with symptomatic heart failure: a contemporary study of prevalence in and characteristics of 700 patients. Oldenburg et al. European Journal of Heart Failure, 2007. View article
Oral Appliances
Oral appliances are a very effective treatment to sleep apnea. Below are several studies that have evaluated oral appliance for effectiveness and compliance.
- The effect of oral appliance therapy on blood pressure in patients with obstructive sleep apnea, Sleep Breath, 2006.
Study: The objective of the study was to investigate the effects of oral appliance (OA) therapy on ambulatory blood pressure in patients with obstructive sleep apnea (OSA).
Conclusion: This study suggests that successful OSA treatment with an OA may also be beneficial to lower blood pressure in OSA patients, as previously suggested for nasal continuous positive airway pressure therapy.
Download article - An Evaluation of a Titration Strategy for Prescription of Oral Appliances for Obstructive Sleep Apnea, Chest, 2008.
Study: We describe the experience of patients treated with an OA, identify factors that predict treatment success with an OA, and offer a protocol for OA titration.
Conclusion: A majority of subjects, regardless of OSA severity, are successfully treated with an OA. Men and younger patients were found to be the best responders. The titration protocol for an OA offers a beneficial initial step in the treatment of OSA.
Download article - Prospective evaluation of an oral appliance in the treatment of obstructive sleep apnea syndrome, Sleep Breath, 2005.
Study: The purpose of this study was to investigate the effects of an oral appliance (OA), with and without mandible advance, in the treatment of obstructive sleep apnea syndrome (OSA)
Conclusion: Oral appliances, especially those that advance the mandible, offer an effective treatment for OSA.
Download article - Role of Oral Appliances in the Management of Sleep Disorders, MJAFI, 2009.
Study: A study was undertaken with the aim to evaluate the therapeutic and clinical efficacy of oral appliances in the management of upper airway sleep disorders like snoring and obstructive sleep apnea (OSA).
Conclusion: Short-term therapeutic efficacy of oral appliances therapy in non-apneic snoring and OSA cases was observed.
Download article - 4-Year Follow-up of Treatment with Dental Appliance or Uvulopalatopharyngoplasty in Patients With Obstructive Sleep Apnea, CHEST, MARCH 2002.
Study: To evaluate the effects of treatment with a dental appliance or uvulopalatopharyngoplasty (UPPP) on demographic variables in patients with mild-to-moderate obstructive sleep apnea (OSA) followed up for 4 years, and compliance and complementary treatment.
Conclusion: The dental-appliance group showed significantly higher success and normalization rates regarding the somnographic variables compared to the UPPP group, but the effectiveness of the dental appliance was partly invalidated by the compliance of 62% at the 4-year follow-up. However, the appliances had few adverse effects on the stomatognathic system and required only moderate adjustments. Use of a dental appliance with regular follow-up can be recommended for long-term treatment of OSA.
Download article - A Randomized Crossover Study of Oral Appliance vs. Nasal-Continuous Positive Airway Pressure in the Treatment of Mild-Moderate Obstructive Sleep Apnea, Chest, 1996.
Study: To compare the efficacy, side effects, patient compliance, and preference between oral appliance (OA) therapy and nasal-continuous positive airway pressure (N-CPAP) therapy.
Conclusion: We conclude that OA is an effective treatment in patients with mild-moderate OSA and is associated with fewer side effects and greater patient satisfaction than N-CPAP.
Download article - A Randomized, Controlled Study of a Mandibular Advancement Splint for Obstructive Sleep Apnea, American Journal Of Respiratory And Critical Care Medicine, 2001.
Study: We aimed to systematically investigate the efficacy of a novel mandibular advancement splint (MAS) in patients with OSA.
Conclusion: The MAS is an effective treatment in some patients with OSA, including those patients with moderate or severe OSA.
Download article - An Oral Elastic Mandibular Advancement Device for Obstructive Sleep Apnea, American Journal Of Respiratory And Critical Care Medicine, 2000.
Study: The first aim of the study was to determine whether a new oral elastic mandibular advancement device (EMA) prevents pharyngeal airway closure during sleep in patients with OSA. The second aim of the study was to determine if the polysomnographic response to the oral mandibular advancement device was dependent on the site of airway closure.
Conclusion: The results show the effectiveness of EMA in the treatment of OSA. The results also indicate that polysomnographic severity of OSA and the site of airway closure should not be used to exclude patients from this oral device treatment.
Download article - Comparison of a Custom-made and a Thermoplastic Oral Appliance for the Treatment of Mild Sleep Apnea, American Journal Of Respiratory And Critical Care Medicine, 2008.
Study: The efficacy of an immediate adaptation of mandibular advancement devices made of thermoplastic material as a treatment option for sleep-disordered breathing (SDB) has been demonstrated in clinical studies. To date, there have been no studies comparing the efficacy of such prefabricated devices with custom-made devices.
Conclusion: In this study, a custom-made device turned out to be more effective than a thermoplastic device in the treatment of SDB. Our results suggest that the thermoplastic device cannot be recommended as a therapeutic option nor can it be used as a screening tool to find good candidates for mandibular advancement therapy.
Download article - Effect of Oral Appliance Therapy on Upper Airway Collapsibility in Obstructive Sleep Apnea, American Journal Of Respiratory And Critical Care, 2003.
Study: We examined the effect of a mandibular advancement splint (MAS) on upper airway collapsibility during sleep in OSA.
Conclusion: In conclusion, we have demonstrated that oral appliance therapy improves upper airway collapsibility during sleep in patients with OSA.
Download article - Mandibular Advancement Device in Patients With Obstructive Sleep Apnea, Long-term Effects on Apnea and Sleep, Chest, 2001.
Study: To evaluate the long-term effects on apneas and sleep and the tolerability of a mandibular advancement device in patients with obstructive sleep apnea.
Conclusion: The long-term effect and tolerability of a mandibular advancement device are good in patients who are recommended the treatment on the basis of a short-term sleep recording, provided that the device is continuously adjusted or replaced with a new one when needed. A short-term follow-up is valuable in the selection of patients who will benefit from long-term treatment with a mandibular advancement device.
Download article
Prevent Sleep Apnea Therapy
Nasal EPAP is an effective treatment option for obstructive sleep apnea. Below are several studies that have evaluated Provent nasal EPAP for effectiveness and compliance.
- A novel nasal expiratory positive pressure (EPAP) device for the treatment of OSA: a randomized controlled trial.
Study: The objective of the study was to investigate the efficacy of a novel nasal expiratory positive airway pressure (EPAP) device as a treatment for obstructive sleep apnea (OSA).
Conclusion: The nasal EPAP device significantly reduced the AHI and improved subjective daytime sleepiness in patients with mild to severe OSA with excellent adherence.
Download article - A convenient expiratory positive airway pressure nasal device for the treatment of sleep apnea in patients non-adherent with continuous positive airway pressure.
Study: While CPAP effectively treats OSA, adherence to CPAP is suboptimal. The short-term efficacy of and adherence with a convenient expiratory positive airway pressure (EPAP) nasal device was evaluated in OSA patients non-adherent with CPAP.
Conclusion: The improvements in AHI and ESS, combined with the high-degree of treatment adherence observed, suggest that the convenient EPAP device tested may become a useful therapeutic option for OSA.
Download article - Predictors of Response to a Nasal Expiratory Resistor Device and Its Potential Mechanisms of Action for Treatment of Obstructive Sleep Apnea
Study: A one-way nasal resistor has recently been shown to reduce sleep-disordered breathing (SDB) in a subset of patients with Obstructive Sleep Apnea Hypopnea Syndrome (OSAHS). The purpose of this study was to examine characteristics predictive of therapeutic response to the device and provide pilot data as to its potential mechanisms of action.
Conclusion: The present study shows that the nasal valve device can alter SDB across the full spectrum of SDB severity. There was a suggestion that subjects with positional or milder SDB in the lateral position were those most likely to respond.
Download article - Long-term use of a nasal expiratory positive airway pressure (EPAP) device as a treatment for obstructive sleep apnea (OSA).
Study: The objective of the study was to evaluate the long-term durability of treatment response and safety of a nasal expiratory positive airway pressure (EPAP) device used to treat obstructive sleep apnea (OSA).
Conclusion: Nasal EPAP significantly reduced the AHI, improved subjective daytime sleepiness and reduced snoring after 12 months on treatment.
Download article - Nasal expiratory positive airway pressure (EPAP) for the treatment of obstructive sleep apnea: a review of clinical studies of proven therapy.
Study: This review is intended to provide healthcare providers with an overview of the available clinical data to support use of this new class of therapy.
Conclusion: These studies have consistently demonstrated that the device is associated with excellent compliance and highly significant reductions in AHI in patients with mild, moderate and severe OSA, including patients who have previously failed CPAP.
Download article - Retrospective case series analysis of a nasal expiratory positive airway pressure (EPAP) device to treat obstructive sleep apnea in a clinical practice.
Study: This retrospective analysis was conducted to evaluate real-world patient acceptance and outcomes of this new therapeutic option in a clinical setting.
Conclusion: EPAP therapy was accepted by 75% of the patients. Use of a chin strap and/or positional therapy in combination with EPAP may contribute to higher effectiveness rates as compared to currently published results.
Download article
A Breakthrough Treatment For Obstructive Sleep Apnea
Nasal Dialator
Nasal dialator can be very effective relief from snoring. Below are a few studies that have evaluated the effectiveness of nasal dialators.
- Effects of the nasal strip and dilator on nasal breathing a study with healthy subjects.
Study: To investigate the effectiveness of nose dialating devices on nasal anatomy and breathing in healthy subjects.
Conclusion: Nasal dialators significantly decreased the cross-sectional area of the nasal valve and decreased nasal resistance. Nozovent dialator proved to be significantly more effective.
Download article - Improved nasal breathing reduces snoring and morning tiredness.
Study:To evaluate the effect a nostril dialator has on patient snoring and tiredness in the morning and to determine how many patients will continue to use the device for 6 months.
Conclusion:The study illustrates the benefits that reducing nasal airway resistance during sleep has on snoring and morning tiredness in patients.
Download article
